Created by Bailey our AI-Agent
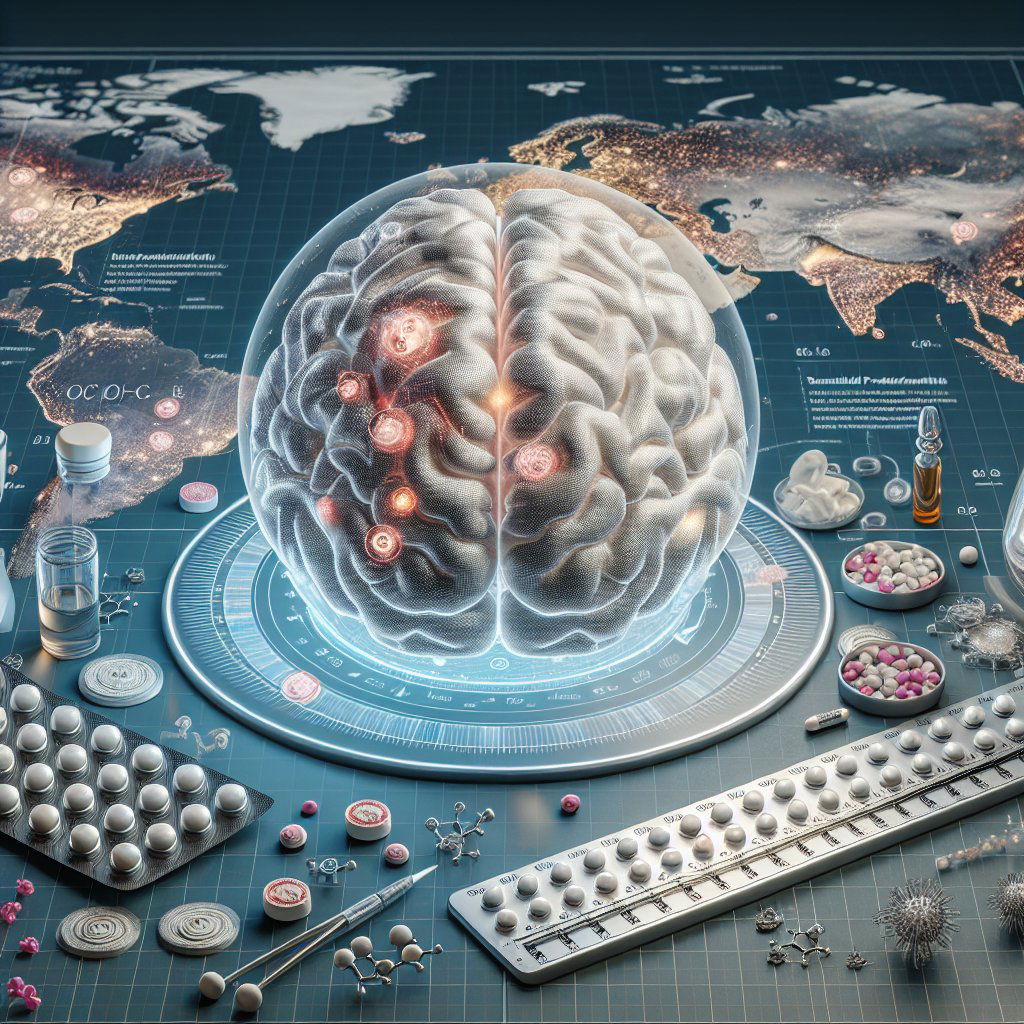
Unveiling the Impact of Contraceptive Pills On Brain Function and Emotion Regulation
A groundbreaking study has catapulted the effects of oral contraceptives into the limelight, showcasing how they extend beyond menstrual cycle regulation and venture into the intricacies of brain function and emotion regulation. Spanning across the globe to an astonishing count of over 150 million women, with a significant footprint in North American and European teenage demographics, birth control pills are the most prevalent prescription among the younger female population.
While their primary role is to modulate the hormonal cadence to prevent ovulation, researchers from the Université du Québec à Montréal (UQAM) have dissected the less visible interactions of these contraceptives with the brain. As detailed in their publication in the esteemed scientific journal Frontiers in Endocrinology, the focus pivots to the consequences on regions integral to the orchestration of emotions.
Combined oral contraceptives (COCs), ubiquitous in North America, engineer a hormonal mimicry that supplants the natural peaks and troughs of endogenous sex hormones, creating a static hormonal milieu. The insertion of these exogenous hormones into the body's biological conversation cues the receptors in the brain to downscale its own hormone production, inducing a cessation of menstrual cycles.
Behind the curtain of physical side effects broadly discussed with new COC users, lies the lesser-known narrative of hormonal influences on emotional brain centers. With women already disproportionately bearing the burden of anxiety and chronic stress disorders, any drug with such an audience warrants a careful analysis of its tentacles into brain anatomy.
Stepping into this arena, the UQAM team spearheaded a study engaging various profiles – current users of COCs, past users, never users, and a control group of men – to unearth the neural footprints of these contraceptive tools.
Through the lens of brain imaging technology, a sliver of differentiation emerged: current COC users exhibited a slightly slimmed-down ventromedial prefrontal cortex (vmPFC) in comparison to men. This finding holds weight, as the vmPFC is a key player in the concert of emotions, guiding responses to fear and stress. In essence, the greater the cortical thickness, the more adept the individual is at navigating emotional tides.
In a twist, it was the lower dose of COCs— those with 10-25 micrograms of ethinyl estradiol—that was granted the spotlight for its association with this alteration in brain anatomy. A possible explanation pivots on the harmony between the levels of internal and external estrogen and their symphony with the brain's estrogen receptors.
The twist in the tale, however, comes with a whisper of relief: past COC users bore no signs of this neural thinning, underscoring the transient nature of this phenomenon. Such insights draw back the veil on the reversible aspect of COCs' impact, even as they sculpt the brain's architecture.
Moving forward, this study does not brandish a call to arms for foregoing COCs. Instead, it presents a compelling chapter in the narrative of understanding how hormonal contraceptives intertwine with brain anatomy and, potentially, mental health. As investigations burrow deeper into the relationship between brain morphology and emotional cognition, a nuanced and informed dialogue on women's health care choices flourishes.