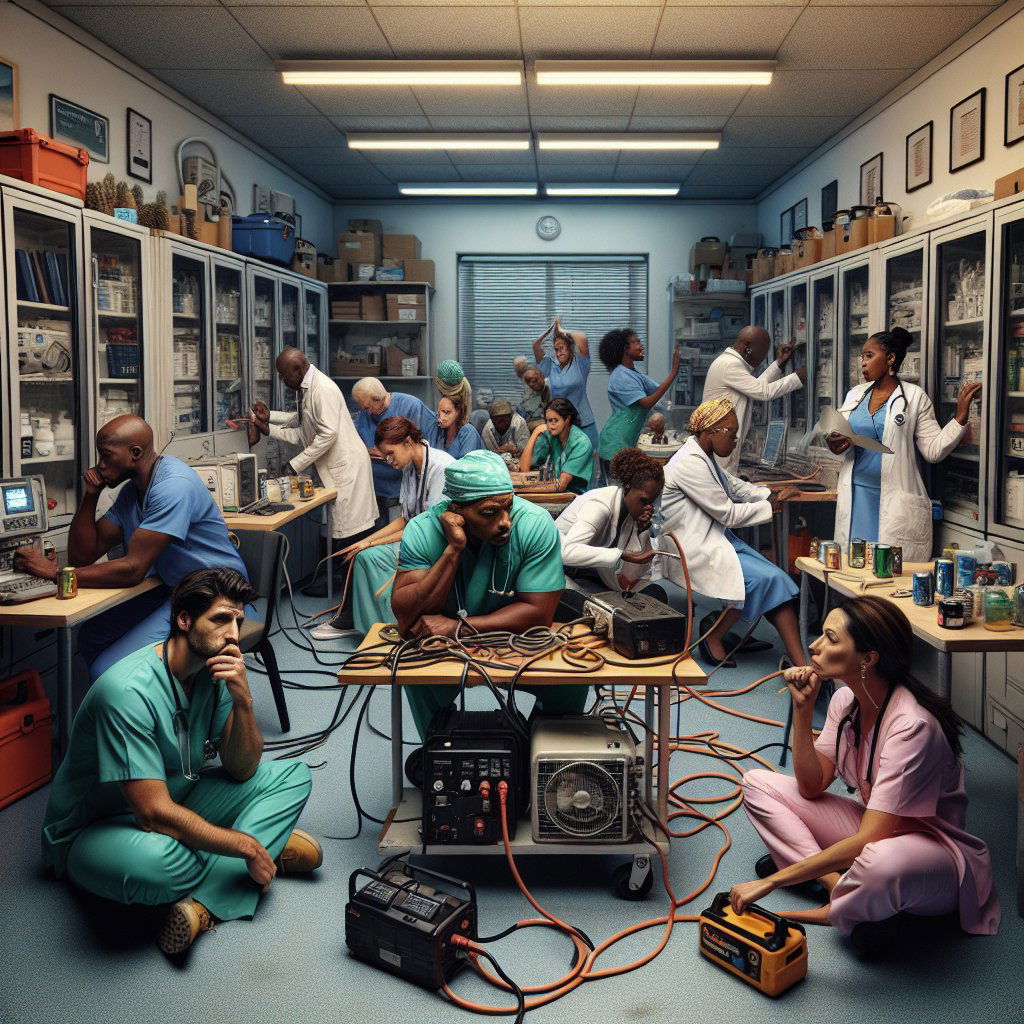
Image: AI generated for illustration purposes
South African Doctors' Mental Health Declining Due to Persistent Load-Shedding, Survey Reveals
In a country where power cuts have become an unfortunate norm, the healthcare sector is feeling an extra layer of strain. A recent survey conducted by the Medical Protection Society (MPS) has shown a worrying trend among South African healthcare professionals, wherein three-quarters of the doctors reported that the ongoing load-shedding has been detrimental to their mental health.
The Medical Protection Society, known for providing medical indemnity cover to healthcare practitioners, conducted the survey with 660 participants. These professionals are grappling with the repercussions of sporadic electricity supply which often leaves homes, clinics, and businesses powerless for up to ten hours a day. The challenge is not minor — load-shedding is threatening the very fabric of South Africa’s healthcare system.
The impact on mental health can't be overstated. The complexities of delivering consistent, quality medical care amidst frequent interruptions in power supply adds to the already high-stress occupation of medical practitioners. But beyond mental strain, these power shortages hold tangible threats to patient safety. Critical medical equipment requires a reliable power source. Without this, the risk of treatment errors, equipment malfunction, and ultimately, harm to patients, escalates exponentially.
Not to mention, the costs associated with running a health-related business in these conditions skyrocket. Generators, alternative energy supplies, and additional contingency plans come at a significant expense. For smaller practices, the financial burden can be debilitating, leading to a decrease in operational hours, staff reductions or even closures — further limiting access to essential healthcare services in various communities.
This situation has brought to light the fragility of the healthcare infrastructure in response to external pressures like load-shedding. Yet, healthcare providers have shown resilience, trying to adapt to the circumstances to maintain patient care. Many have turned to backup power solutions and streamlined procedures to stay functional during blackouts. However, these are temporary and often expensive stopgaps — not sustainable solutions.
The government's efforts in tackling the power crisis appear sluggish when matched with the urgency called for by professionals at the healthcare frontline. To prevent a worsening of the healthcare crisis, investments and expedited actions in energy infrastructure are crucial. Moreover, establishing a more robust means for hospitals and clinics to operate independently of the unstable grid could be a life-saving directive.
The MPS report serves as a call to action for immediate intervention to protect not only the mental health of doctors but also the well-being and safety of patients across the country. As South Africa grapples with power instability, its effects ripple outward, making the role of the government and energy sector critical to the immediate pursuit of stability and long-term solutions.